

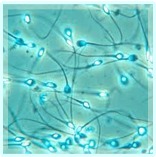
Infertility affects approximately 15% of all couples, and male factors contribute to approximately half of these cases, with no identifiable cause in 25%. “Male factor” infertility is seen as an alteration in sperm concentration and/or motility and/or morphology in at least one sample of two sperm analyses, collected between 1 and 4 weeks apart (World Health Organisation, 1999).
 There are a wide range of causes of and treatments available for male infertility. Understanding the cause can help determine which treatment should be offered, whether this be an operation to try and bypass a blockage in the tubes carrying the sperm, or a procedure to retrieve sperm surgically from the testicles to be used subsequently in IVF and ICSI. Oliver Wiseman works together with the experienced team at the world famous infertility clinic, Bourn Hall Clinic, to offer patients the full range of options and help couples to maximize their chances of having a child.
There are a wide range of causes of and treatments available for male infertility. Understanding the cause can help determine which treatment should be offered, whether this be an operation to try and bypass a blockage in the tubes carrying the sperm, or a procedure to retrieve sperm surgically from the testicles to be used subsequently in IVF and ICSI. Oliver Wiseman works together with the experienced team at the world famous infertility clinic, Bourn Hall Clinic, to offer patients the full range of options and help couples to maximize their chances of having a child.
These can be due to problems with manufacture of the sperm in the testes (non-obstructive), or due to a blockage of the transport of sperm after their production (obstructive). It is important that men with absent or low sperm numbers are thoroughly investigated, to ensure that:
The manufacture of sperm can be affected by a number of problems. These can be:
There are several causes for blockages of the sperm carrying tubes (epididymis and vas), which can result in male fertility problems.
A varicocoele is a collection of dilated veins which surround the testicle. They may visible when the patient stands up, and may cause discomfort or aching. They more often develop on the left hand side rather than the right. The link between varicocele and fertility is much debated. Varicoceles are present in 30 to 40 per cent of men who experience fertility problems, but many men with the condition are able to conceive without problems. Correction of the varicocoele may lead to improvement in sperm number and quality, but whether this translates into improved pregnancy rates in unclear.
It is important that the couple are treated together, and that female factors such as age and any gynecological history are taken into account.
In men where these is no obvious cause for low sperm numbers or lack of sperm in the ejaculate, surgical sperm retrieval (SSR) can be used. This can be either PESA (percutaneous epididymal sperm aspiration) or TESE (testicular sperm extraction). Oliver Wiseman works with the fertility experts and embryologists at Bourn Hall Clinic and regularly performs these procedures in conjunction with this expert team, and is well placed to discuss which is most suitable for you, and the likely success rates. The sperm retrieved would then be used for ICSI, which is a form of IVF where a single sperm is injected into a single egg to make an embryo. Oliver offers patients who require SSR due to poor sperm production micro TESE (miscrosurgical testicular sperm extraction). This technique allows individual areas of the testicle to be inspected under the microscope, and only those areas where the tubules are dilated and thus more likely to contain sperm are removed to look for sperm. In this way the chances of finding sperm are higher, and the amount of testicular tissue removed is much less, thus helping to preserve the testicle ability to make testosterone, the male hormone. Please contact us for more details about micro-TESE.
In men where there has been an obstruction to the flow of sperm, one option is to try and correct this. If there has been a previous vasectomy, then vasectomy reversal would be a possibility, and this is performed using microsurgery. For more information please click here . If the nature of the blockage is such that success from repair is thought to be low, or the time since the vasectomy is so long that reversal is unlikely to be successful, then Oliver can discuss the possibility of surgical sperm retrieval, either PESA or TESE (see above).
Visit our News page to read articles about male infertility issues from the Cambridge Urology Partnership team.
Read an article by Oliver Wiseman in Fertility Road magazine